MAKEAWARE!
Data pills and workshops to raise awareness on antibiotic consumption and antimicrobial resistance
PROJECT DESCRIPTION
MAKEAWARE! is a four-year initiative (2022–2025) developed at the Institute of Design (IDe) of the University of Applied Sciences and Arts of Southern Switzerland (SUPSI). The mission of the project is to raise public awareness and actively involve citizens in the fight against Antimicrobial Resistance (AMR) through interactive, data-driven activities designed to foster participation, dialogue, and understanding.
The project adopts a design approach and methodology to make complex health issues, such as antimicrobial resistance (AMR), tangible and understandable. A dedicated research framework, developed in collaboration with experts in science, technology, and communication, supports the creation of creative, hands-on workshops accessible to everyone. These activities invite participants to share experiences, reflect on treatment practices, and consider everyday behaviours related to antibiotic use. Active participation supports a bottom-up approach to generating and interpreting data, transforming lived experiences into valuable insights for public health. All methods, tools, and results are shared in this open repository to encourage further experimentation and expand the dialogue on the topic of antibiotic consumptionmption and resistance. MAKEAWARE! is part of SPEARHEAD, an Innosuisse-funded project involving a consortium of eight public and four private Swiss institutions addressing AMR from multiple perspectives. SPEARHEAD (Swiss Pandemic & AMR Health Economy Awareness Detect) applies a multidisciplinary, research-driven approach that combines digital tools with a citizen-centred focus, promoting responsible use of antibiotics through prevention and stewardship.
What is antimicrobial resistance?
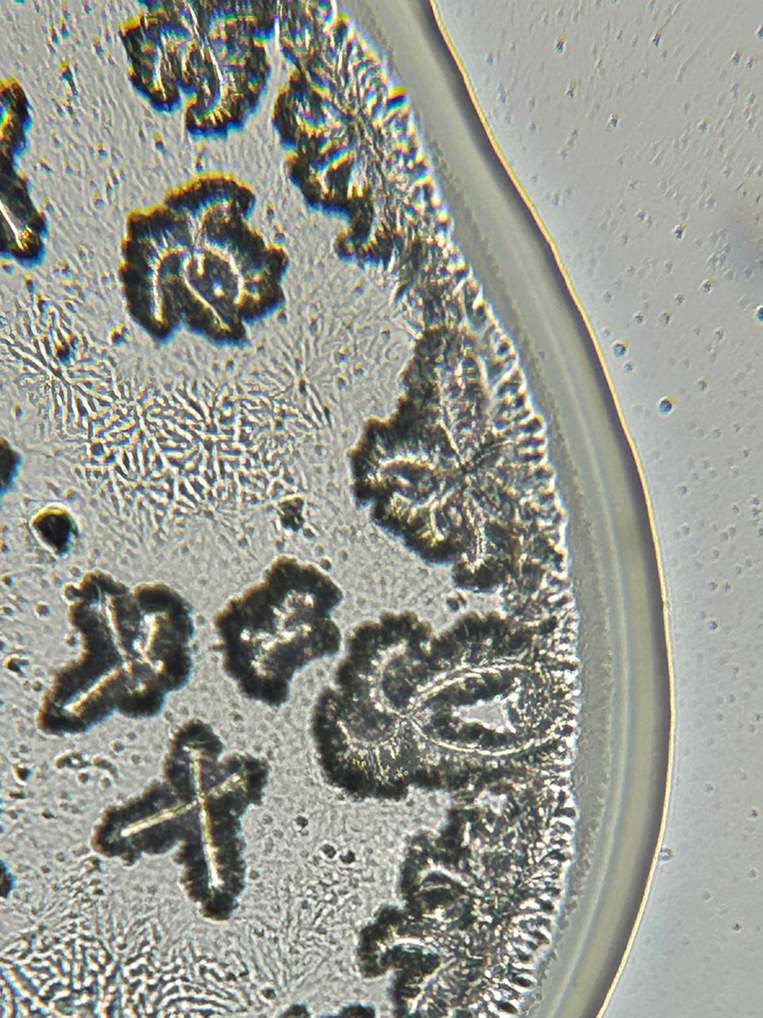
Antimicrobial resistance (AMR) describes the capacity of microorganisms — including bacteria, viruses, fungi, and parasites — to survive exposure to medicines designed to kill them or stop their growth. These medicines, known as antimicrobials, include antibiotics (for bacterial infections), antivirals (for viral infections), antifungals (for fungal infections), and antiparasitic agents (for parasitic infections). When microorganisms develop resistance, standard treatments lose their effectiveness. Infections then persist for longer periods, may spread more easily, and can require alternative or more intensive therapies. This reduced effectiveness complicates infection control, increases the risk of severe illness, and can contribute to higher healthcare costs and mortality (WHO, 2023).

Microbial resistance to antibiotics is a natural survival mechanism that enables microorganisms to adapt and withstand external threats. While resistance can emerge gradually through genetic changes, its spread has been accelerated by the widespread and often inappropriate use of antimicrobials. Human-driven factors — including poor hygiene, inadequate infection control in healthcare environments, and the misuse of antibiotics in agriculture and the food supply chain — have amplified the problem far beyond clinical settings (EU Commision, 2025; CDC, 2025).
Antimicrobial resistance currently presents serious risks to food safety, global trade, and the effectiveness of routine medical procedures such as surgeries and chemotherapy. The World Health Organization (WHO) recognises antimicrobial resistance as one of the top ten global public health threats (WHO, 2023).
The MAKEAWARE! initiative focuses on bacterial resistance to antibiotics, a specific type of antimicrobial resistance, and aims to bring attention to the issue and create debate to improve public understanding of human antibiotic use. The project explores consumption habits and treatment practices to raise awareness and promote more responsible behaviours, including avoiding unnecessary antibiotic use, completing prescribed courses, and refraining from taking medication intended for others.
How many resistant bacteria have been detected Worldwide?
Hundreds of bacterial species worldwide have developed resistance to one or more types of antibiotics, reducing the effectiveness of treatments and limiting options for controlling infections. The World Health Organization’s 2024 Priority Pathogens List recognises 24 bacteria that have already shown documented resistance to multiple types of antibiotic treatment (WHO, 2024).
Global surveillance has documented resistance in hundreds of bacterial species, showing a widespread adaptation to antimicrobial drugs. Antibiotic classes—such as penicillins, cephalosporins, macrolides, tetracyclines, and fluoroquinolones—share similar structures or modes of action but differ in use. Resistance to one or more of these classes limits treatment options and complicates infection control. The WHO’s 2024 Priority Pathogens List names 24 resistant bacteria across 15 families, ranked as critical, high, or medium priority. Many of the most urgent threats are Gram-negative bacteria, whose additional protective cell wall layer makes them harder to treat. This barrier can block certain medicines, sometimes requiring broad-spectrum antibiotics that act against many bacteria. While useful in emergencies, frequent or unnecessary use of these drugs can accelerate resistance. Narrow-spectrum antibiotics target specific bacteria and help slow resistance, but may be less suitable when the exact cause of an infection is unknown.
Resistance develops within the bacteria, which adapt through genetic changes to withstand medicines that previously proved effective. Resistant bacteria are not linked to specific individuals but represent a collective public health challenge. Once resistance develops, these strains can spread between humans, animals, and the environment, often without causing symptoms in carriers (O'Neill, 2016; WHO, 2025).
In Switzerland, resistance appeared in 158 of 1,958 tested bacterial samples in 2019, reflecting a rate of approximately 8%. These resistant strains circulate across hospitals, communities, farms, and natural environments. Infections caused by these bacteria are estimated to contribute to about 300 deaths annually, underscoring the urgency of coordinated prevention and control efforts across healthcare, agriculture, and environmental management (FOPH, 2025).
Which geographic region has the highest number of resistant bacteria in Switzerland?
Switzerland shows moderate levels of antibiotic resistance compared to other European countries, with higher rates in French- and Italian-speaking cantons such as Geneva, Ticino, and Vaud. These areas generally record greater antibiotic use than German-speaking regions like Zurich and Bern, partly due to differences in prescribing habits and healthcare practices (FOPH, 2025).
Antibiotic resistance in Switzerland reflects both its geographic position and socio-cultural diversity. At the European level, Switzerland occupies an intermediate position, with resistance rates lower than in neighbouring countries such as Germany, France, and Italy, but higher than those observed in Nordic nations. This moderate level is shaped by a combination of prescribing habits, healthcare practices, and public attitudes toward antibiotics. Within the country, regional differences in language and culture influence patterns of antibiotic use and resistance. Surveillance data show that French- and Italian-speaking cantons, including Geneva, Ticino, and Vaud, typically report higher antibiotic consumption compared to German-speaking regions such as Zurich and Bern.
These differences arise from variations in outpatient prescribing practices, healthcare culture, and patient expectations.
Higher antibiotic use in these areas increases opportunities for bacteria to develop resistance, which contributes to relatively elevated resistance rates. While national surveillance captures overall trends, more localised monitoring would help design region-specific strategies for promoting responsible antibiotic use and reducing resistance
(Anresis, 2024).
What is the impact of antimicrobial resistance in the future?
Antimicrobial resistance (AMR) threatens to make many infections harder, or even impossible, to treat. Without action, modelling scenarios suggest global deaths could reach around 10 million per year by 2050, surpassing cancer as the leading cause of death. These figures are based on projected outcomes that assume current trends continue without significant intervention. To date, approximately 1.27 million people die each year from drug-resistant infections, with AMR contributing to nearly 5 million deaths overall (GBD, 2021).
Antimicrobial resistance poses a serious and growing threat with wide-ranging consequences for individuals, healthcare systems, and society. As bacteria become resistant to antibiotics, infections require longer treatment, more complex care, and often prolonged hospital stays. This increases the emotional and physical burden on patients and their families while driving up healthcare costs through the need for alternative medicines and intensive medical support (Murray et al., 2022). The effects extend beyond healthcare, influencing daily life, economic productivity, and long-term health outcomes. In severe cases, resistant infections can lead to permanent disability or death. Modelling scenarios that assume current trends continue without major changes in prevention and treatment suggest that AMR could cause around 10 million deaths each year by 2050 (O'Neill, 2016).
In this projection, resistant infections would surpass cancer as the leading cause of death worldwide. These figures are not certainties but illustrate the potential magnitude of the problem and the consequences of inaction.
All credible assessments point to the need for coordinated global action. Strengthening surveillance, improving infection prevention, promoting responsible antibiotic use, and investing in new treatments remain essential to prevent AMR from escalating into a large-scale public health crisis.
Although estimates differ due to the complex nature of the issue, the overall trend highlights
the urgent need for a coordinated and global response to prevent antimicrobial resistance from
developing into a major public health crisis
(WHO, 2019).
When did the lack of antibiotics start?
Most antibiotics in use today were discovered over 30 years ago, and very few entirely new types have been developed since. Since 2017, only 12 new antibiotics have been approved, most of which belong to existing classes, making them vulnerable to the same resistance mechanisms as older drugs (WHO, 2021).
The slowdown in antibiotic discovery began decades ago and has contributed to a growing shortage of effective treatments. Most antibiotics currently in use are based on discoveries made more than 30 years ago (WHO, 2021). Since 2017, only 12 new antibiotics have been approved, and the majority of these belong to existing classes—groups of antibiotics that share similar chemical structures and mechanisms of action. When bacteria become resistant to one antibiotic in a class, they often gain resistance to others in the same group, reducing treatment options and highlighting the urgent need for novel drug classes (CDC, 2024). The development of new antibiotics faces significant challenges. Scientific obstacles include the difficulty of finding compounds effective against resistant bacteria, while economic barriers stem from limited financial incentives for pharmaceutical companies.
Drug development is often directed toward medicines with quicker commercial returns, leaving antibiotic research underfunded (O'Neill, 2016). Some studies are exploring non-antibiotic alternatives, such as preventive treatments for urinary tract infections, but these approaches are not yet sufficiently effective for widespread medical use (Advani et al., 2025; Çelik et al., 2025 ). Recent advances in drug discovery methods offer some promise. In 2023, researchers used artificial intelligence (AI) and advanced computational screening to identify zosurabalpin, a new antibiotic with activity against Gram-negative bacteria that are common in hospital-acquired infections. This breakthrough demonstrates how innovative research approaches can open new possibilities for antibiotic development (David et al., 2021).