WORKSHOPS
15 September, 2024
HEK, Basel
Perturband Fluids
w/Zoe Romano
Perturbant Fluids workshop aims to enhance and disseminate bodily autonomy and rethink possible relationships with the "perturbing" entities that embody us. During this workshop participants will be involved in the discovery of scientific protocols and tools to redefine the way we can contribute and redesign the narrative around science.
9 August, 2024
Fab24 Mexico
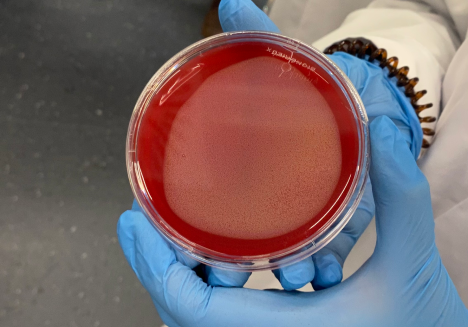
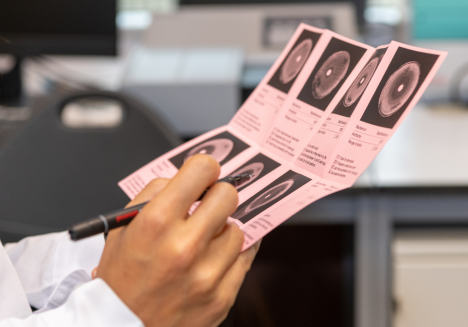
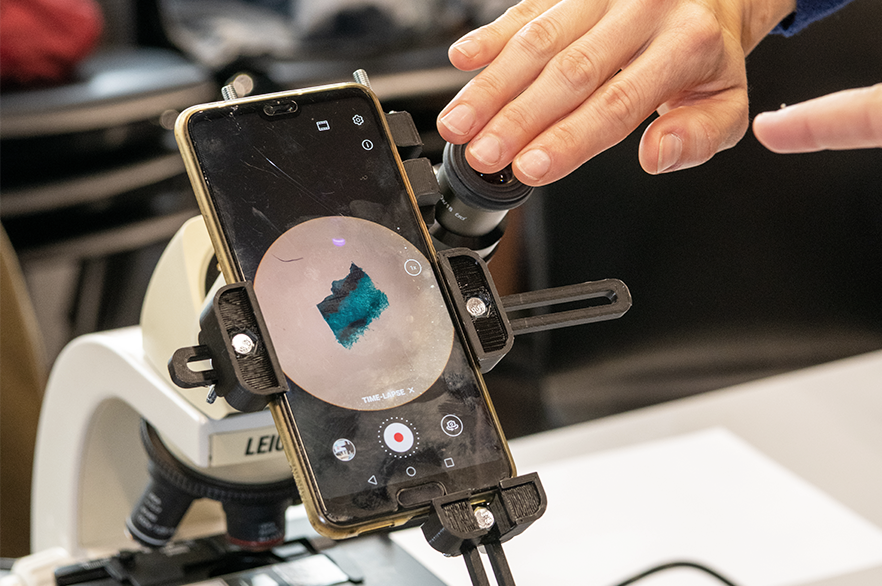
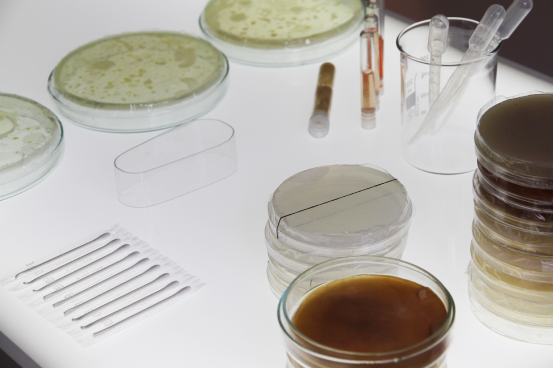
DipLab - Digital Petri Laboratory
w/ Matteo Subet

This workshop offers participants an exciting opportunity to deepen their understanding of antibiotics and antibiotic resistance through the digitization of the antibiogram test, made possible outside of microbiology laboratories. Attendees will be able to broaden their knowledge of antibiotics and antibiotic resistance, and explore the role of these life-saving drugs in modern medicine.
TBD
-
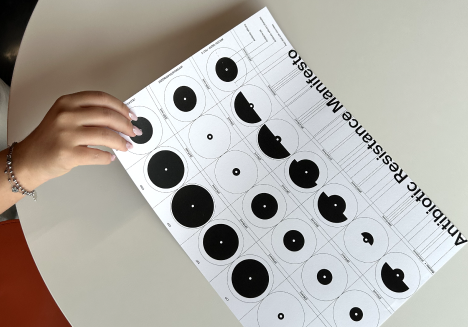
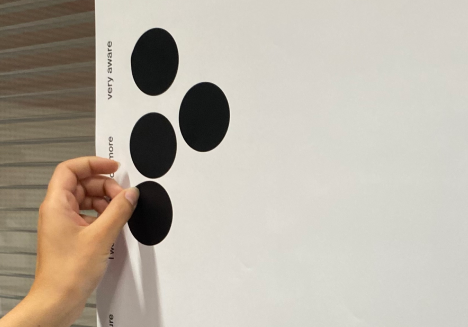
Visualizing the Resistance
w/ Cristina Corti

This workshop proposes an hands-on experience to learn and discover the science around antimicrobial resistance. Starting from scientific contents, the activities will engage the participants in the creation of a collaborative repository of images, resources and stories that will help contributing to the fight against antibiotics misuses and its consequences.
Past
Basel
OneHealth Datathon
at Novartis Pavillon

Antimicrobial resistance is a global threat that directly or indirectly affects each and every one of us. On the 21st of June, people who experienced antimicrobial resistance, together with healthcare professionals, will be working supported by designers to envision possible technology solutions to the challenge of resistance development.
Past
-
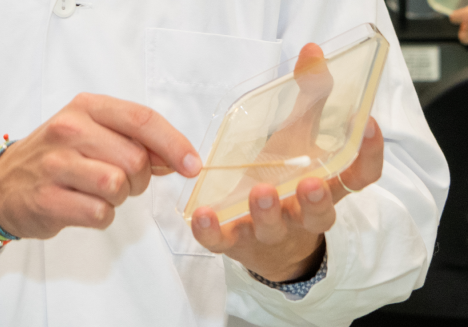
Biofilie Lab
w/ Isabel Farina & Giulia Tomasello
This workshop proposes an hands-on experience to learn and discover the science around antimicrobial resistance. Starting from scientific contents, the activities will engage the participants in the creation of a collaborative repository of images, resources and stories that will help contributing to the fight against antibiotics misuses and its consequences.
TBD
-
Shape your Symptoms
w/ Ginevra Terenghi
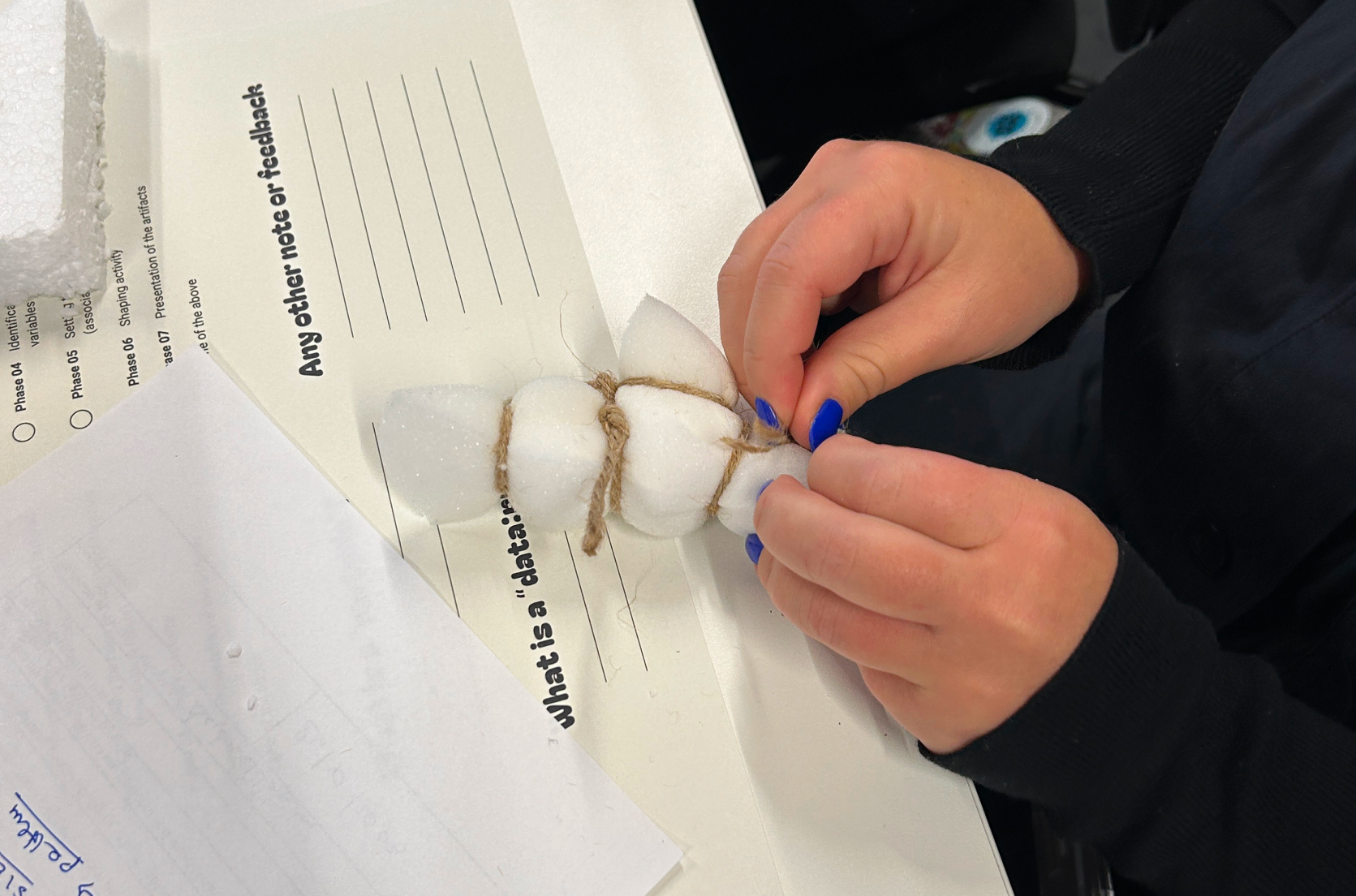
Are you a women and suffer from urinary tract infections (UTIs)? Have you ever experienced urinary tract infections, such as cystitis, or are you chronically affected by this sort of diseases? Did you have any troubles with the treatment? Was the antibiotic not effective or did it cause side effects? Take part in this workshop to support the research.
Past activities
21.06.24
OpenHealth Datathon
MAKEAWARE! team
Novartis Pavilon
Basel, CH
10.06.24
DiPLab - Digital Petri Laboratory
Matteo Subet
SUPSI
Mendrisio, CH
24.05.24
Shape Your Symptomps
Ginevra Terenghi
SUPSI
Mendrisio, CH
18.05.24
Perturbant Fluids
Zoe Romano
OBOT Project
La Rada
Locarno, CH
02.05.24
Shape Your Symptomps
Ginevra Terenghi
Brunel University London
London, UK
30.04.24
DiPLab - Digital Petri Laboratory
Ginevra Terenghi
SSMT
Locarno, CH
27.03.24
DiPLab - Digital Petri Laboratory
Matteo Subet
Liceo Cantonale
Locarno, CH
01.12.23
DiPLab - Digital Petri Laboratory
Matteo Subet & Antonella Autuori
Kantonsschule Zürcher Unterland
Bülach, UK
24.11.23
Biofilie Lab: Growing vaginal microbiome at home
+ more info
Isabel Farina & Giulia Tomasello
SUPSI, FabLab
Mendrisio, CH
23.11.23
Perturbant Fluids
Zoe Romano
OBOT Project
ImpactHub Ticino
Lugano, CH
27.09.23
Visualizing the Resistance
Cristina Fragoso
Applied Microbiology Lab
SUPSI, FabLab
Mendrisio, CH
26.09.23
Visualizing the Resistance
Cristina Fragoso
Applied Microbiology Lab
SUPSI, FabLab
Mendrisio, CH
12.05.23
Visualizing the Resistance
Cristina Fragoso
Applied Microbiology Lab
SUPSI, FabLab
Mendrisio, CH
18.03.23
Perturbant Fluids
Zoe Romano
OBOT Project
Onl'fait
Genève
05.12.22
Visualizing the Resistance
+ read the articlePamela Principi, Cristina Corti Fragoso
Applied Microbiology Lab
SUPSI, FabLab
Mendrisio, CH
11.11.22
Perturbant Fluids
+ read the articleZoe Romano
OBOT
SUPSI, FabLab
Mendrisio, CH